FROZEN SHOULDER
If you suffer from severe pain caused by frozen shoulder, please Schedule an appointment with one of our orthopedic specialists as soon as possible.
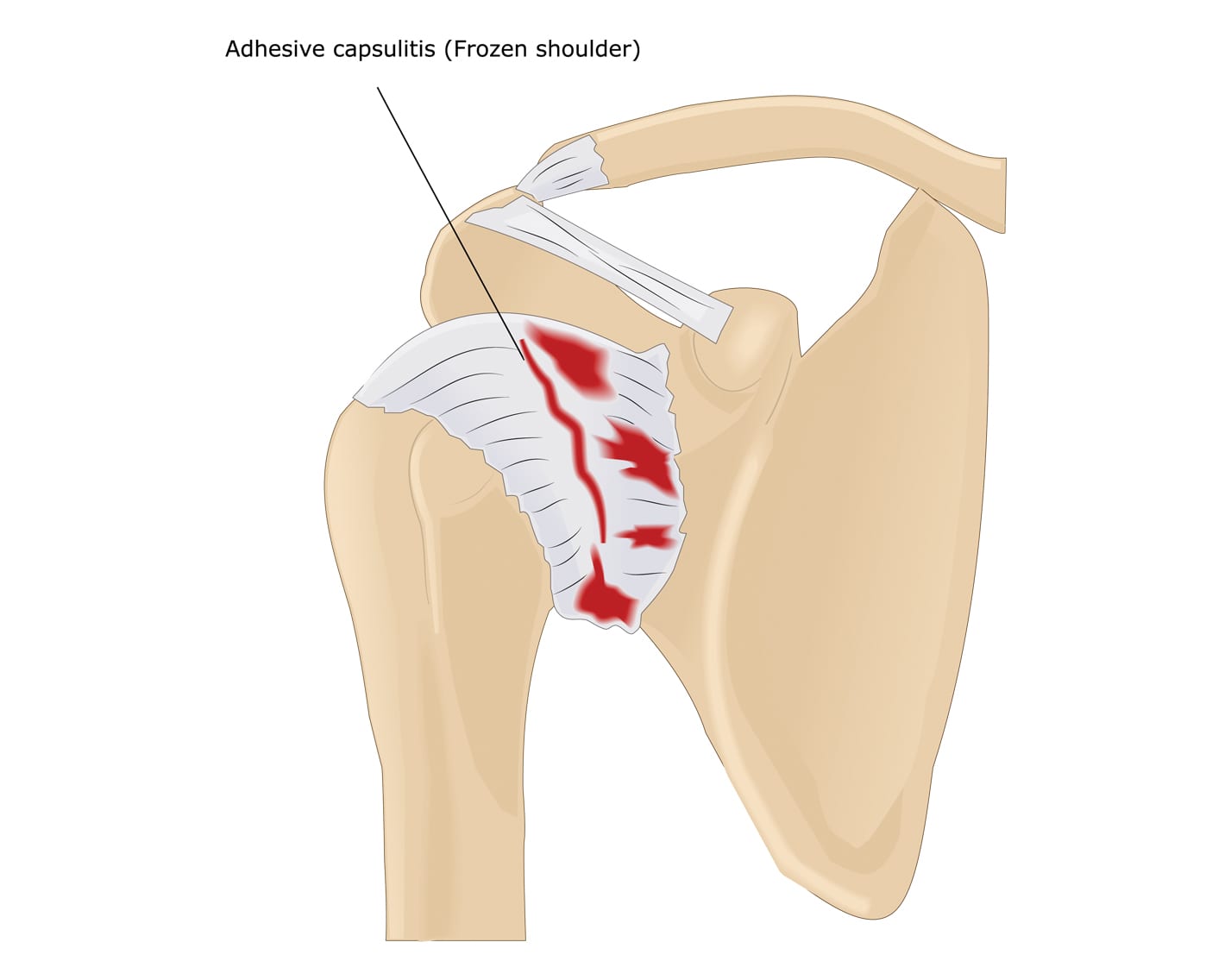
Adhesive Capsulitis, also known as Frozen shoulder, causes stiffness and pain in the shoulder joint. Signs and symptoms typically start small and gradually worsen over time and then resolve themselves, usually within one to three years.
The risk of developing a frozen shoulder increases if you have recently recovered from a medical condition or procedure that prevents you from moving the arm — such as a stroke or a mastectomy.
Treatment for a this condition usually involves performing range-of-motion exercises and sometimes corticosteroid injections and numbing medications injected into the joint capsule. In a small percentage of cases, shoulder specialists may recommend arthroscopic surgery to loosen the joint capsule so that it can move freely.
While unusual for frozen shoulders to recur in the same shoulder, some people may still develop it in the opposite shoulder.
Symptoms of a Frozen Shoulder
A Frozen shoulder will typically develop slowly, over the course of three stages. Each stage may last a number of months.
- The Freezing stage. Moving of the shoulder will cause pain, and the shoulder’s range of motion starts to shrink.
- The Frozen stage. Pain may diminish during this stage. However, the shoulder will feel much stiffer, and much more difficult to move.
- The Thawing stage. The range of motion in the shoulder will slowly improve.
For some people, the pain worsens at night, making it difficult to sleep.
Causes of a Frozen Shoulder
The bones, ligaments and tendons that make up the shoulder joint, sit inside a protective capsule of connective tissue. Frozen shoulder occurs when this capsule thickens and tightens around the shoulder joint, restricting its movement.
Doctors find cases of Adhesive Capsulitis tend to occur more often in people who have diabetes or those who recently had to immobilize their shoulder for a long period, such as after surgery or an arm fracture.
Treatment options for Frozen Shoulder
When treating frozen shoulder, controlling shoulder pain and maintaining as much range of motion in the shoulder as possible remain the top priorities.
Some treatments for Frozen Shoulder include:
Medications
Pain relievers such as aspirin and ibuprofen can help reduce pain and inflammation. Your provider may prescribe stronger pain-relieving and anti-inflammatory drugs depending on the severity of the injury.
Physical Therapy
Physical therapists diagnose and treat patients with medical problems or injuries that limit their ability to take part in their daily lives. Patients will usually see a physical therapist after a referral by their primary physician. Physical therapists work with patients who have experienced an injury or disease that has affected their movement and range of motion.

